Herniated Disc
Overview
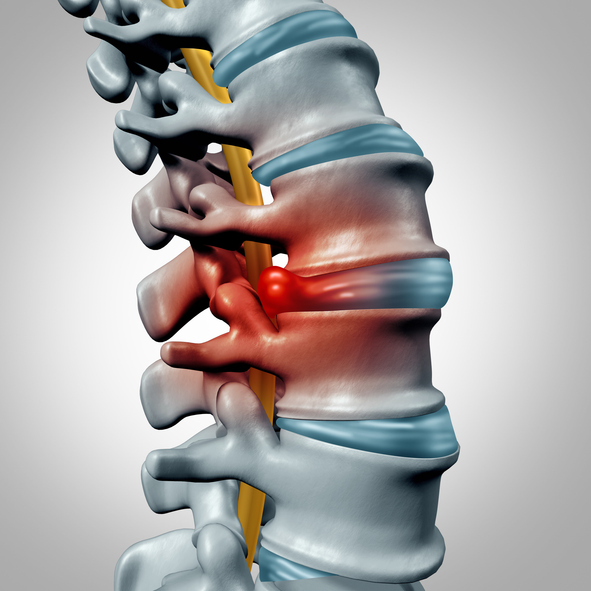
A herniated disc, also called a slipped disc or ruptured disc, occurs when the soft inner material of the disc pushes through a tear in the tough outer layer. This can irritate nearby nerves, causing pain, numbness, or weakness in an arm or leg. Herniated discs most often occur in the lower back (lumbar spine), but they can also occur in the neck (cervical spine).
Symptoms
Common symptoms of a herniated disc include:
- Arm or leg pain, depending on which disc is affected
- Numbness or tingling in the body part served by the affected nerves
- Muscle weakness that can affect your ability to lift or hold items
- Pain that worsens with certain movements or positions
- Pain that improves with certain positions or rest
Causes
A herniated disc can be caused by:
- Age-related disc degeneration (discs become less flexible and more prone to tearing)
- Lifting heavy objects with improper technique
- Twisting and turning while lifting
- Being overweight, which puts extra stress on discs
- Genetic predisposition to disc degeneration
- Physically demanding occupations
- Traumatic injury that causes disc damage
Diagnosis
Diagnosing a herniated disc typically begins with a thorough physical examination and medical history. Your doctor will check your muscle strength, reflexes, walking ability, and sensitivity to touch. Imaging tests like MRI scans provide detailed images of your spine and can confirm the location and severity of disc herniation.
Diagnostic Methods
- Physical examination
- Medical history review
- Neurological examination
- Imaging tests (MRI, CT scan, X-rays)
- Nerve conduction studies
Treatment Options
At Southeastern Spine Institute, we offer comprehensive treatment plans tailored to your specific condition and needs.

Conservative
Most herniated discs improve with conservative treatment, including rest, physical therapy, pain medication, and anti-inflammatory drugs. Your doctor may recommend limiting activities that cause pain and gradually introducing gentle exercises.

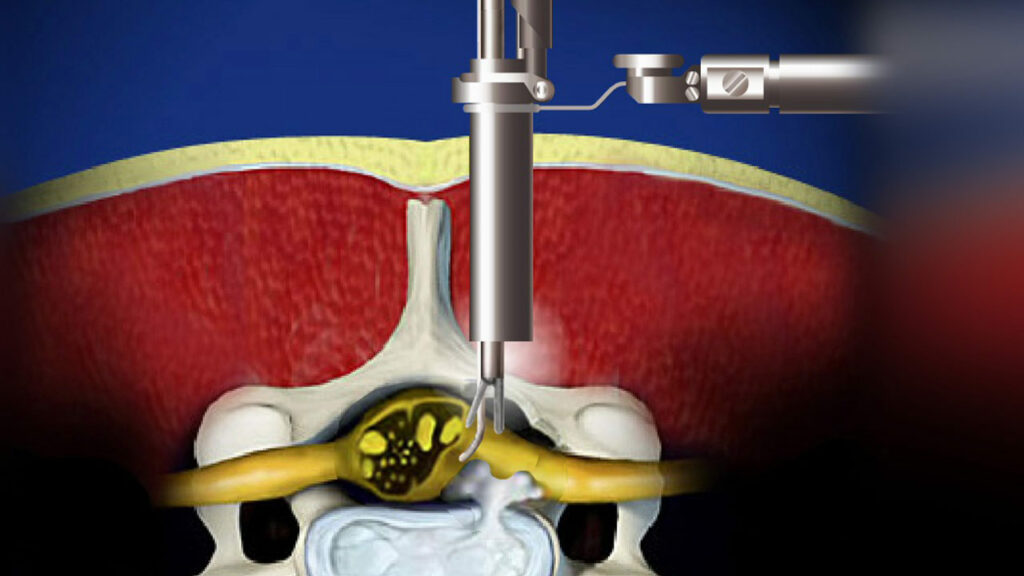
Non-surgical Procedures
Epidural steroid injections can help reduce inflammation and pain by delivering medication directly to the affected area. These injections can provide temporary relief while the disc heals naturally.

Surgery
If conservative treatments don't improve symptoms after 6-8 weeks, or if you have severe weakness or difficulty walking, surgery might be recommended. Common procedures include microdiscectomy (removing the protruding portion of the disc) or in rare cases, disc replacement.
Frequently Asked Questions
Can a herniated disc heal on its own?Yes, many herniated discs heal on their own over time. The body can gradually reabsorb the herniated portion of the disc, which can reduce pressure on nearby nerves and alleviate symptoms. This natural healing process typically takes several weeks to months.
How long does it take to recover from a herniated disc?Recovery time varies depending on the severity of the herniation and individual factors. Many people experience significant improvement within 4-6 weeks with conservative treatment. Complete recovery may take 1-3 months, while some cases may require longer healing periods.
Can I prevent a herniated disc from occurring?While you can't prevent all herniated discs, you can reduce your risk by maintaining good posture, using proper lifting techniques, staying physically active, maintaining a healthy weight, quitting smoking, and avoiding prolonged sitting.
Will I need surgery for my herniated disc?Most people with herniated discs don't require surgery. Approximately 80-90% of patients improve with conservative treatment. Surgery is typically considered only when conservative treatments fail, or when there are progressive neurological symptoms or severe pain.
Don't Let Spine Pain Control Your Life
Our team of spine specialists at Southeastern Spine Institute is dedicated to helping you find relief and return to the activities you love.